Case history 2
September 21, 2021
"This is online E log book to discuss our patients de- identified health data shared after taking his or her guardian's signed informed consent hear we discuss our individual patients problems through a series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs.This E log book also reflex my patient centered online learning portfolio and your valuable inputs on comment box is welcome."
A 55 yr old male patient presented to OPD with chief complaints of fever associated with chills since 5 days , weakness of right upper limb & left lower limb since 4 days , B/ L knee pain, abdominal distension, facial puffiness, bilateral pedal edema, giddiness, loss of appetite ,loose stools .
PRESENT HISTORY:
Patient was apparently asymptomatic before one week then he got fever which is low grade intermittent & associated with chills.
Pain in abdomen ( umbilicus).
No vomitings,headache,cough.
No decreased urine output.
Burning sensation during micturition is positive.
No history of seizures, renal issues.
PAST HISTORY:
No history of diabetes mellitus , hypertension, TB , asthma , CAD, CUA.
Patient tested positive for covid 8 months back.
Patient has a history of trauma 2 years back and the treatment was given by placing an implant on right hand.
Patient had history of typhoid, liver issues one year back which were subsided with medication.
No history of renal problems.
PERSONAL HISTORY:
Appetite- lost
Diet - mixed
Sleep - adequate
Bladder movements - normal
Bowel movements - black stools
Addictions - chronic alcoholic & chronic smoker ( chutta).
Family history
No history of similar complaints in family.
General examination :
Patient is conscious, coherent, cooperative.
No pallor
No icterus
No cyanosis
Edema of feet - present ( bipedal edema)
VITALS:
Temperature - 100.4 F
Respiratory rate - 18 / min
Pulse rate - 63/ min
SpO2 - 97 %
SYSTEMIC EXAMINATION:
CVS:
No thrills
No cardiac murmurs
S1 S2 heard.
RESPIRATORY SYSTEM:
Breath sounds- vesicular
No wheeze
No dyspnea
ABDOMEN:
No palpable mass
No tenderness
Hernial orifice - normal
No bruit heard
CNS:
No neck stiffness
Level of consciousness- Alert
Speech- normal
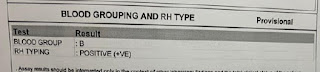
INVESTIGATIONS:
ABG test
Hemogram






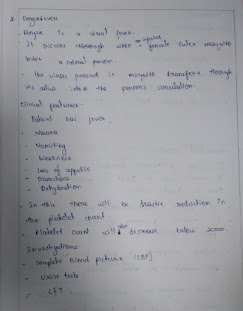
Comments
Post a Comment